

George Manos lies on the bed at an independent living facility in Rocky Hill, Connecticut. Manos is 86 years old and began struggling with the effects of dementia in his early eighties.


Leandra Manos helps her father out of the van after an evening out doing errands. George’s doctor recommended he stop driving at 81 after early cognitive testing and a car accident.
has spent nearly three years as the full-time caregiver for her 86-year-old father, George Manos, who is in the later stages of dementia. Dementia and COVID have given Leandra the battle of her life. Leandra’s journey has left her without full-time employment as she works to protect and care for her father. The rising prevalence of dementia is becoming a worldwide crisis requiring more research and better long-term care provision. According to Alzheimer’s Disease International, “Over 55 million people worldwide lived with dementia in 2020.’’

was sitting down and sort of in a daze but speaking freely. The words came out, but they weren’t right. ‘Dad, I have your pills for you.’ ‘Are these the files?’ ‘Yes, these are the files.’ ‘Ok, they need to be copied to (some specific – I have no clue) folder.’ ‘Yes, I did that; they’re all set.’ He nods, satisfied. ‘So here are your pills. Open your mouth.’ He complies, and I give him his pills.
Sometimes he's off-topic, but it makes sense if you know where his train of thought is. Obviously, his word supply wasn't on the pills but on his employment as a computer programmer that ended 35 years earlier. Other times, he makes no sense at all. It is a lovely mixed-word salad. I play along as a parent would do when their baby babbles seriously. It’s a beautiful thing to try to communicate, irrespective of age or success. Just as a baby’s effort in trying to communicate is worthy of their parent’s full attention and acknowledgment, so is an elderly parent’s effort to communicate with their adult children. To focus on the frustration the listener may feel in not knowing what in heaven’s name they’re talking about is small.
Dad feels bad upon realizing he’s not being understood. My heart sinks for him when we’re in a small group setting with two or three people talking and laughing, and dad’s listening jovially; he says something to engage in the conversation when suddenly, everyone stops talking because someone asked him, ‘What? What do you mean?’ It’s like the flow has been interrupted, and now the focus is on him, hurting him because he can’t think of the right words to explain what he means. When this happens in my presence, I deflect the nonsensical comment and say something like ‘I know, right?!’ and just continue with whatever is being said so he feels heard and his mood matches that of the conversation. He feels good. There’s nothing he can do about it, so why make him feel bad?
Sometimes Dad unknowingly makes up words, thinking they are words. I already must pay super close attention to him because I’m deaf (I have neuro-sensory hearing loss), and when he’s making up words, often speaking just above a whisper, it’s difficult to know if it’s his brain or mine not working properly.
We became ‘roomies,’ as I like to say, on April 4, 2020. One day earlier, on April 3, 2020, Dad was about to be discharged from the hospital after a five-day stay due to a UTI left untreated too long. His Assisted Living facility did not inform me that something was wrong until too late. My daily visits to him had ceased two weeks prior due to the new pandemic visitation rules, so I’d been separated from Dad leading up to hospitalization. Except for his time in the ER before admission, I was separated from him there, too. I remember speaking to the hospital doctor about his discharge, being told that dad was very weak, his muscles had atrophied, and they strongly recommended short-term rehab upon discharge. My gut told me he’d die of the coronavirus if I sent him for rehab, as he barely survived a UTI due to pandemic hysteria and resulting policy changes (no family visitation, change in internal operations such as no community meals, no social activities, etc.).

Over the last two years, Leandra Manos has had many close calls when her father, George, has gotten out of bed and wandered around at night. Her solution is to sleep next to his bed to prevent him from hurting himself.
‘Can I bring him home?’ I asked the doctor. ‘You can bring him home,’ he replied, ‘but caring for him will be difficult. It won’t be easy.’ He reinforced this very kindly over and over to ensure I understood. I was getting a new version of my dad back, not the old one. ‘Yes, I know,’ I told him. ‘I’ll try. I think I can do it.’ The next day, I rented a pickup truck, loaded it with a hospital bed I found on Marketplace, then got Dad. He could barely stand, let alone walk. He didn’t talk. I took a deep breath as I watched two staff try to get him into the truck, and realizing he could not speak, I held his hand as I drove an hour home.
Caregiving is hard and requires a lot of strength to persevere. I learned this firsthand when, after several years of decline, my mother became bedridden with multiple sclerosis (MS) in the fall of 1992 while I was in my senior year of high school. Dad was her primary caregiver for 12 more years at home before she was placed in a nursing home and passed away about a year later. I helped Dad as often as possible: in junior high and high school, on college breaks, and when I moved back home after graduating. So, I had some decent exposure to caregiving. When caring for dad, though, I had the advantage of 20/20 hindsight, knowing how things went with my mom. I knew exactly what I wanted to be done differently, particularly when it came to taking care of myself as a caregiver.
In 1996, I was on a visit home from college. I always loved my visits home, even though Mom’s MS was getting worse. She was bedridden and declining, having noticeable difficulties speaking, and was starting to have trouble swallowing. Care was around the clock, repositioning her in bed every two hours, and Dad was then what I am now… a full-time caregiver for our loved one. I walked into the front door of our three-story colonial and went into our former dining room, which had turned into Mom’s bedroom. Dad was on one side of the bed, and I was on the other. I was giving my parents all my collegiate news from the last time I saw them a few months prior. Beyond my father, I saw some weird, discolored, dried-up gunk on the wall in the corner behind the grandfather clock.
I continued my chatter with them, all the while noticing the gunk. An hour later, I asked Dad, ‘What’s that on the wall?’ ‘Applesauce,’ he said, looking away before he told me the story. He was trying to give my mom her meds, and she wouldn’t swallow. He lost his patience, got mad, and threw the applesauce, which splattered onto the wall. I didn’t say much. I knew he was one of the most caring people, but I also knew that Mom’s condition was a test of patience. ‘I’m sure she couldn’t help it, Dad,’ I said. ‘I know,’ he said. That dried applesauce stayed on the wall for probably another 15 years. It served as a constant reminder to me that despite all the love in the world we have for our loved one, all the patience, all the effort, all the absolute everything that caretakers put into caring for their family member, tempers will fly, patience will run out, anger will rage, exasperation may set in. And in caring for my dad, I can say that it is true. Within a year after spending over $6,000 renovating my bathroom, I almost punched my fist through the beautiful new wall when I nearly lost it on Dad. I probably almost ripped the sink off the pedestal at some point (thank goodness I failed to do that). Caretaking is challenging and can push even the most patient, loving caretakers to the brink. To deny that is to deny the truth

Leandra and George light a candle at the Saint Spyridon Greek Orthodox Cathedral. The candle is lit in memory of a recently departed relative.
However, what is lost is gained elsewhere. As an around-the-clock caregiver, you must find ways to be positive in the face of the inevitable negatives. When Dad’s speaking word salad, not being understood, I appreciate his communicating with me. When he asks if I’ve spoken to Leandra lately (I am Leandra), I feel his love for me, content that I am in his head and heart. When I’m wiping his rear end and cleaning his privates due to incontinence, I am grateful to be the first person to see and address any concerning spots or redness that might not be relayed to me immediately if someone else were caring for him. When he’s weak for several days and unable to walk far, it makes ‘good days’ when he can take a short stroll more memorable and meaningful. When it takes three hours to get him ready for the day, from when he’s woken for his first set of meds until he’s finished his first meal, I can instead be thankful that we have seen a new morning.
Recently, on Orthodox Good Friday, it took me two hours to get him dressed and ready to go to evening services at church. I had been to this church before, but it was not our ‘home’ church and not one I frequented. Nevertheless, it was the closest one to us, and due to the time pinch, it was the only one we could get to on time. After the three-hour service, we got back into the car, and I asked him if he was glad we went to church. ‘Yes, I really am.’ After a pause, he asked, ‘Did you like the service?’ ‘It wasn’t bad,’ I said. ‘What did you like about it?’ he asked. ‘To be honest, dad, what I liked most about it was that you were with me. I love you.’



Leandra Manos smiles while showing her “Baba” his shirt for the day. Leandra converted her front room into a living space for her father, George, allowing him to easily access the kitchen and bathroom. She rents out the home’s second story to help her pay the bills.

Leandra has a daily routine with her father, and she bathes and dresses him in the morning to prepare him for the day.
Early on, the two used to manage the routine well together.

Leandra feels responsible for her father. She says, “That he took the time to raise me and that nobody can care for him as I can.”
.png?crc=328676584)
Leandra Manos pauses during her exercise class in Manchester, Connecticut. Manos occasionally pays for a caregiver to
look after her father while she tends to her necessities.

Leandra Manos and her father, George, sit quietly in the sanctuary of St. Spyridon Greek Orthodox Cathedral in Worcester, Massachusetts. George and the family attended the church for many years.

George waits in the van's passenger seat as Leandra runs into the house to get his medication that must be taken on schedule.

Leandra says her final goodbyes to Tiki before the vet euthanizes her beloved pet. Her 14-year-old dog, Tiki, has cancer and has not eaten much in several weeks. Manos is a lover of animals; she has two dogs, two cats, a rabbit, and nearly a dozen chickens.
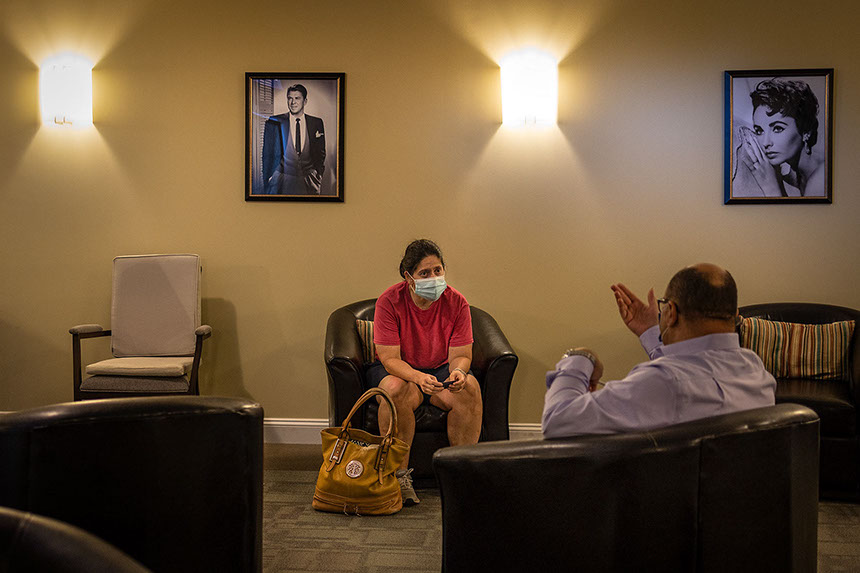
As COVID restrictions loosen, Leandra visits a memory care facility to learn more about the cost of long-term care. After discovering it would cost her between $8,000 and $10,000 per month, she leaves disappointed.

Overcome by her circumstances, Leandra sits on the front porch. One of George’s home healthcare providers unexpectedly stopped seeing George.
Daily chores and yard work have been all but unattainable over the last two years because of her father’s constant needs.


A note from Leandra:
Education is at the heart of my purpose in sharing our story. I’ve always been committed to learning and teaching. As a college student, I gravitated toward educational programs that offered hands-on internships. As a patient, I gravitate toward teaching hospitals (volunteering to be the guinea pig, if you will). As a daughter, I commit to working directly with and teaching every aide who assists my father for at least two weeks, often longer. It takes an incredible amount of sacrifice. However, in any situation, the sacrifice yields the best result in developing the most skilled and competent practitioners.
Caring for a loved one with dementia is still a somewhat closeted topic. Most people don't talk about it openly. However, once you start caring for a loved one with dementia, you slowly become connected to others who have done so or are doing so now. Before you know it, you realize there's an entire continent of people struggling desperately, being decimated in every facet of their lives (financial, social, emotional, spiritual, environmental, physical, and intellectual), and nobody is talking about it. There aren’t enough government or private programs to support families in all locations. Also, there isn’t enough funding to support the existing programs, resulting in a nearly futile program offering that exists only in theory, with no practical application.
Until our collective voices are heard statewide and nationwide, enough to encourage legislative and systemic changes in how our elderly are cared for and supported by their loved ones, we must be the proverbial ‘picketers’ for our family members. My solution in my little bubble of just one patient, my father, is to rewrite a book of solutions or, rather, to expand on a few suggestions. To get through the challenges of caring for a loved one with dementia, I have had to think outside the box and generate creative proposals. Yet with change comes some pushback. When I reach out with a new idea to someone who can potentially help, I get one of two responses: ‘That's ingenious! That's amazing! I've never heard of that before! Let’s try! Let’s see how I can help!’ or ‘Can’t do that, that's not how it's done. Impossible. Nope, it won't work. Can’t help you.'
I share this story to inspire and help others in the same position. I want to bring awareness to this issue to help brainstorm, unite, offer support, and systemically change our status quo. As a society, we can do better—and we must—not only for my dad but also for you and your loved ones.
Selected awards and film festivals in 2022–23:
“The Long Goodbye, A Caregiver’s Journey,” Documentary Film, 26:45, directed/produced/cinematography by Steven G. Smith
National Press Photographers Association, The Northern Short Course, Best of Show, Long-Form Multimedia, March 2023
• The Best of Photojournalism Contest 2022: Honorable Mention – Documentary Film, Feb. 2023
• Brussels World Film Festival: Semi-finalist – Best Short Documentary, Feb. 2023
• National Press Photographers Association, The Northern Short Course: First Place – Long Form Multimedia, Feb. 2023
• Tokyo Shorts Film Festival: Winner – Best Human Rights Film, Jan. 2023
• Denver Movie Awards: Semi-finalist – Best Documentary, Jan. 2023
• Athens International Art Film Festival: Finalist, Special Mention – Best Documentary, Dec. 2022
• European Cinematography Awards (ECA): Semi-finalist and Best Cinematography, Nov. 2022
• Praque Underground Film Festival, Semi-Finalist, Best Documentary Short, Nov. 2022
• Mannheim Arts and Film Festival: Winner – Best Human Rights Film, Oct. 2022
• Berlin Shorts Award: Semi-finalist – Best Documentary, Oct. 2022
• New Filmmakers New Orleans: Semi-finalist – Best Documentary, Sept. 2022
“The Long Goodbye, A Caregiver’s Journey,” Picture Story:
• STAT, An intimate look at dementia — and its emotional toll on family and caregivers, March 2022
https://www.statnews.com/2023/02/28/dementia-emotional-toll-family-caregivers/
• Pictures of the Year International: Finalist – Best Issue Reporting Story, April 2022
• National Press Photographers Association, The Northern Short Course: First Place – Picture Story, May 2022
• National Council on Aging: Second Place, June 2022
Educational Programs and Dementia Care Resources:
Alzheimer's and Dementia Caregiving, Alzheimer's Association, https://www.alz.org
National Institute on Aging (NIA), National Institutes of Health, https://www.nia.nih.gov/health/caregiving/advance-care-planning
Nancy Mace and Peter Rabins, The 36-Hour Day: A Family Guide to Caring for People Who Have Alzheimer’s Disease
Louis Theroux, director, Extreme Love: Dementia, 2012, https://www.bbc.co.uk/programmes/b01gvt26
Acknowledgements:
A special thank you to Leandra and George Manos for graciously sharing their story.
"This project is in love and dedication to my father, who suffers from dementia, and my mother, who is his caretaker."
– Steven G. Smith, producer and filmmaker
About the Producer:
Steven G. Smith’s work focuses primarily on the art of visual storytelling and filmmaking. He enjoys working collaboratively on films and new media projects to utilize each team member’s strengths. His passion is telling stories that can impact the community. He aims to be a sensitive, compassionate storyteller who believes in community engagement and giving subjects agency. To contact him, please reach out to him at steve@stevengsmith.com. Steve teaches visual storytelling at the University of Connecticut.

Contact 970 618 5584 Email: steve@stevengsmith.com